“5 Tips to Make IVF Easier” | myMindBodyBaby
First, let’s be clear. Making the decision and proceeding with an IVF cycle is never going to be easy. But it is our hope that in understanding these 5 Tips to Make IVF Easier we can help make the process a little less stressful.

A decision not to be taken lightly
Deciding to proceed with IVF is a big decision. It requires a physical, mental, emotional – not to mention, financial – investment. In fact, all things considered, it may be one of the biggest decisions you’ve had to make. Given this, understanding the ‘ins and outs’ of IVF seems prudent.
Making things a little easier
Many clinics require you to attend an information session before proceeding with IVF. While these sessions can provide a lot of information and answers – they may also leave you feeling overwhelmed. There are so many variables, options, and outcomes associated with IVF. You may leave the session knowing you need to proceed down this path – but feeling lost in the numbers and details. So without further ado, let’s take a look at 5 Things Tips to Make IVF Easier and how they can better prepare you to face this next step in the journey to grow your family.
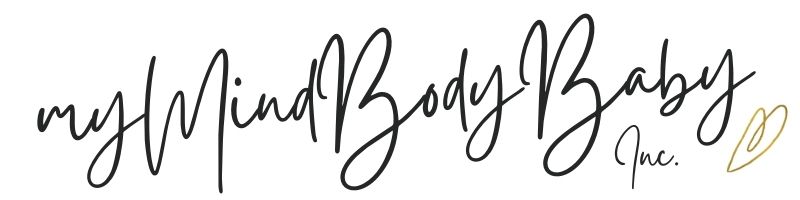
Tip #1 Understand your timeline and specifics
Once you make the decision to proceed with IVF you may feel rearing to go. Let’s get this started! But it is important to be realistic about the timelines and details.
The timeline
You may be required to undergo some preliminary investigations and testing before beginning your IVF cycle. These often take place on specific days of your cycle. So if you make the decision to proceed with IVF in, say January, you may not be able to complete all of the initial testing and procedures until your next cycle in February. If you’re lucky and are able to review the results of your tests with your doctor before your next cycle begins, you may be able to begin the medication for IVF in the next month (March – in this example). If it takes a few weeks for the results to come in and for an appointment, with your doctor you might be looking at the following cycle to begin medication.
Medications vary depending on your approach
Generally, IVF will require a variety of formats of medications:
- Oral
- Injectable
- Vaginal
- Anal suppositories
- Dermal patches
Not everyone will require all options, but it is important to know that these options may be involved.
Traditional IVF (we will look at “mini IVF” later) generally has two protocol options: the long protocol option (also called “Long Agonist” and a shorter protocol (usually referred to as an “Antagonist” approach). FertilityIQ does a great job of explaining the differences in this article. Each protocol has certain medications associated with it.
What happens when?
The medication schedule for your cycle will vary depending on the approach your doctor believes will maximize your success rate. Most clinics will set up an appointment for you to speak with a nurse about all of the different medications and what your specific timeline looks like. The nurse will show you how to administer the different medications and which medications require refrigeration. The window of time to take most of the medications is quite specific – and so it is important to determine what will work best for you. For example, if you have the option – is it easier for you to administer injections in the morning (before work) or in the evening? Will you be able to give yourself the injection or do you think you will need your partner or a support person to help you? This may impact the timing of medication. Some people find it helpful to have a specific IVF journal to help keep track of meds, timings, and questions for your next appointment.

It’s a numbers game
The medications will stimulate your ovaries to mature more follicles than you would during a normal menstrual cycle. But this isn’t a game of the more the merrier. Your healthcare team is aiming for a sweet spot in terms of eggs to be retrieved. Too few, and your odds of success are reduced. But too many – and the quality of those eggs retrieved may be reduced and your risk of OHSS is increased (more on this later).
The success rates of IVF – and by success, we mean the end result being a live birth – vary greatly depending on your specifics. Your age, genetics, physical health, underlying conditions, and other factors all play a role in the quantity and quality of eggs retrieved, fertilized, and leading to the delivery of a healthy baby.
The rough math
Let’s take a look at general numbers. A fertility doctor is usually aiming for 15-20 mature follicles. From these, they expect roughly 75% to have eggs available to be retrieved – so about 12-15 eggs. Of those eggs retrieved, about 70% will usually fertilize leaving 8-10 embryos. About 40% will make it to the cellular stage where they can be transferred or frozen – which gives you 3-4 embryos. If you opt to genetically test your embryos (more on PGS testing later) then 50% may come back “normal” – leaving you 1-2 embryos for transfer. Most clinics are now opting to transfer 1 embryo per transfer and the success rates of implantation and subsequent pregnancy leading to live birth varies based on all of the variables mentioned above – but is often quoted at a 60% pregnancy rate.
What are your risks?
Understanding the general, and your specific, risks are important in helping you prepare for your IVF cycle. There are standard risks associated with each medication and your healthcare team will outline these for you in your introduction session. There are also risks that you may be more prone to – like ovarian hyperstimulation syndrome (OHSS). OHSS is when your ovaries are overstimulated from the medication, causing them to become very swollen. OHSS occurs only after the eggs are retrieved and if the fluid from the swollen ovaries leaks into your abdominal and surrounding cavities. While the rate of OHSS is low (3-6%) certain factors are known to increase your risk:
- Being younger than 35
- Using injectable medications to stimulate follicular maturation
- Patients with PCOS
- High levels of estrogen during fertility treatments
Your healthcare team will identify any risk factors and will monitor all patients for risk factors of OHSS throughout the cycle. If you are deemed at higher risk for OHSS your healthcare team may discuss a frozen embryo transfer during a subsequent menstrual cycle as pregnancy resulting from a fresh transfer can further increase the risk of OHSS (pregnancy causes estrogen levels to further increase).
Tip #2 Understand your options
The basics of IVF are as follows:
- Use medication to prompt your ovaries to produce more mature eggs than you would otherwise.
- Retrieve the increased number of eggs.
- Fertilize the eggs in a laboratory using your partner or donor sperm.
- Transfer a fertilized egg.
- Test for pregnancy.
And while this may sound simple, you may be presented with a number of different options in addition to the basics.
ICSI
What is it?
Intracytoplasmic sperm injection, or ICSI, is when a single sperm is injected directly into an egg. For a more in-depth look at ICSI check out this article, guest written for us by an embryologist.
When is it used?
ICSI is often recommended when there are low sperm numbers, issues with sperm motility, if the sperm has been retrieved from the testes vs. ejaculated or if there have been previous issues with fertilization during IVF.
How much does it cost?
Depending on your clinic ICSI can cost an additional $800-$2,500 CAD.
Mini IVF
What is it?
Mini, micro, or minimal stimulation IVF are the terms used for an IVF cycle where the goal is to produce a smaller number of eggs using less medication, or in some cases no stimulation medication. As with a standard round of IVF you would still be monitored throughout the cycle, the egg(s) would still be retrieved and fertilized in the lab and then the resulting embryo would still be transferred back into your uterus.
When is it used?
It is used in a few different circumstances.
- OHSS – If you are at high risk of OHSS you may want to be less aggressive with the medications
- If you are taking medication for cancer and your aim is to preserve eggs – stimulation medication may exasperate the cancer progression
- Cost -if this is a concern – fewer drugs mean reduced costs
- With low ovarian reserves – the increased drugs may not help mature more eggs, meaning the cost of the increased medications may be wasted
How much does it cost?
A standard IVF round costs roughly $12,000 – $15,000 CAD (this price is dependent on the coverage you may have and the options you proceed with) and a mini or micro IVF is approximately half the cost.
Effortless IVF
What is it?
Effortless IVF uses INVOcell to incubate the embryo, versus incubation happening in a lab. The steps are the same as for standard IVF (medication to stimulate ovaries, eggs retrieved, eggs fertilized) but then the fertilized egg(s) are placed in the INVOcell back into the woman’s uterus.
When is it used?
- To reduce the costs – as incubation is not happening in the lab there are cost savings associated with this procedure
- Same-sex couples – called “reciprocal IVF”. One partner can proceed with the IVF cycle and INVOcell incubation, and the second partner can then opt to have the embryo transferred to her uterus to proceed with the pregnancy.
What does it cost?
The cost is roughly half the cost of a standard IVF cycle.
PGS
What is it?
Pre-impanation genetic screening, PGS, is a genetic test performed on the fertilized egg to test for chromosomal abnormalities. Unlike pre-implantation genetic diagnosis, which looks for specific gene defects you may know you are at risk for, PGS tests for a standard spectrum of common genetic abnormalities.
When is it used?
PGS is often recommended when if you have had subsequent rounds of IVF that have failed or you have experienced multiple miscarriages.
What does it cost?
PGS costs an additional $3,000-$7,000. Costs vary per clinic and as some testing facility charge a flat rate for up to a certain number of embryos some patients will opt to proceed with multiple retrieval rounds to have enough embryos to test. PGS also impacts your timelines: embryos must be frozen, you wait for the results to come back, and then you would transfer a “normal” embryo during a subsequent cycle.
Tip #3 Be your own advocate
Your fertility journey is very unique to you. No two journeys are alike. Your path to parenthood is going to impact your emotions, your mental health, your body, your relationship, and your finances differently than it would the person sitting next to you in the clinic waiting room. You will also be faced with different choices along your road and you will be forced to make decisions. For all of these reasons we firmly believe self-advocacy is a key factor in helping make this process easier.
What does “self-advocacy” mean?
It means speaking up for yourself – communicating to your partner, support circle, and also importantly your healthcare team about how you are feeling and any concerns you are having. Question your options like ICSI, PGS, frozen vs. fresh transfers and medication formats to ensure you are doing what is best for you and your family. It also means listening to your gut. Try to be clear on your goals and how far you are willing to go. It means being able to say, “We have had enough.”
Asking tough questions
It can be difficult to know what questions to ask. And sometimes, even when you know what questions to ask, it can be intimidating to ask them. We have created a free tool to help you outline your personal goals, identify your individual concerns + a list of common questions to help you get started having those conversations with your healthcare team.
Tip #4 Know what support looks like for YOU
The free, downloadable workbook in the link above will help you to outline some of your questions and concerns. It should also help you to think about what type of support will make this cycle easier for you. For example – do you need help with your medications? Your nurse may be able to administer some. You may also find it easier for a friend or partner to perform the injections. Other areas to think about:
- If you haven’t shared with your friends or family that you are struggling with fertility, will opening up about your journey make the process easier on you?
- If you do not want your extended social circle to be aware of the journey you are on, do you have a close confidant you can lean on? Check out this article on the benefits of having this type of support throughout your journey.
- Would seeking professional support benefit you? Some clinics have on-site counselors. You can also find support through organizations like Healing Infertility or Lighthouse Fertility & IVF Coaching.
Tip #5 Know you are doing everything you can
Finally, at points, you may feel like you’re not doing enough. That there must be something else you can do to increase your chances of success. If you are following your medication schedule and taking care of your mind and body know that you are doing everything you can to lead to a successful outcome.
Taking care of your body
Taking care of yourself physically means ensuring proper nutrition and exercise. Proper nutrition ensures you are fuelling your body with the right nutrients to sustain you through this journey and creating the optimal environment for pregnancy. Did you know that research has shown that a Mediterranean style diet (think high in veggies, legumes, nuts, and good fats) has been shown to support higher IVF pregnancy rates? This is precisely why our recipes and meal plans are based on a Mediterranean approach to nutrition.
Proper exercise ensures you are giving yourself a stress outlet during this harrowing journey, promoting beneficial blood flow and helping to release mood-boosting endorphins. Did you know research has shown that regular, moderate exercise leading up to an IVF cycle can actually increase your chances of success?
If you are looking for a more in-depth program – complete with a full meal plan, recipes, day-by-day exercise program, and mental well-being tools like meditations and positive visualizations – you can check out our IVF Fitness & Nutrition Guide here.
Finally – make sure you keep following along with us on Instagram and Pinterest! Plus, you can gain additional support through our Private Facebook group. We provide daily tips, inspiration, and support – like “What to Eat The Night Before Your IVF Transfer” (click the image to get the recipe!) – to help guide you along your journey.