“Implantation: How Does it Happen and What Can You do to Support it?” | myMindBodyBaby
If you’re here, visiting us at myMindBodyBaby (your online hub for all things fertility-related!), you probably have two big questions on your mind today:
- What is going on in my body during the two-week wait (TWW)?
- What can I do to increase my chances of a fertilized egg implanting in my uterus?
So let’s dig in!
Your Body During the TWW
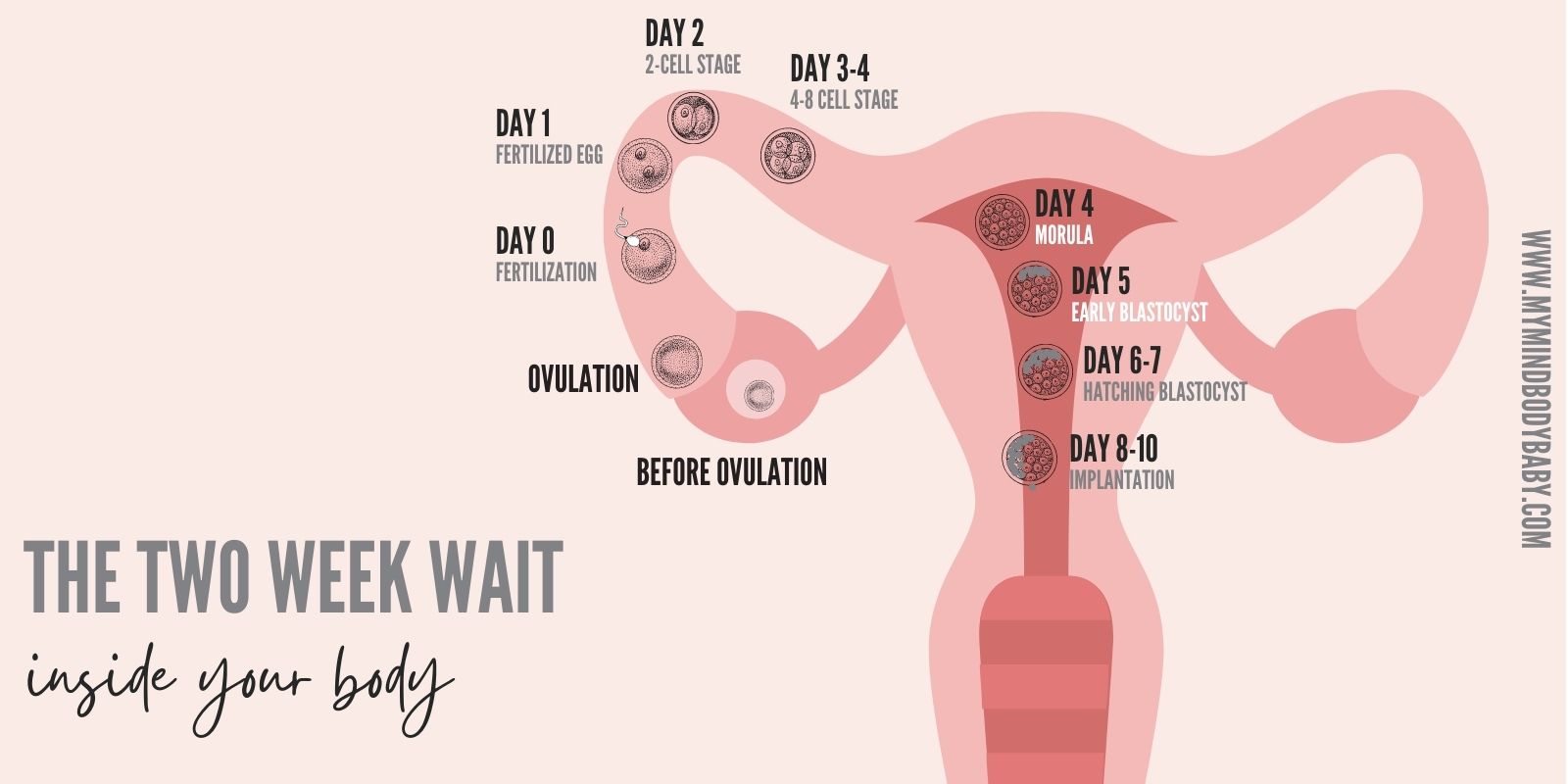
The two-week wait starts at ovulation and ends when you either get a positive pregnancy test or your period begins. But let’s back up to the beginning of your cycle.
After your period, the start of which marks the beginning of your cycle, your uterine lining responds to your increasing levels of estrogen by thickening (for a full breakdown of what goes on each month read this). Your ovaries respond to your fluctuating hormone levels and release a mature egg. If you have timed intercourse properly (or you’ve done a round of IUI) the egg has a chance of being fertilized.
Fertilized or not, the ovulated egg will travel down the fallopian tube to your uterus where your uterine lining continues to change to become more receptive to implantation. Surging progesterone levels further prepare the lining to receive a fertilized egg. It generally takes about 8-10 days for a fertilized egg to implant into the uterine lining.
What is needed for implantation?
Implantation can occur when a fertilized egg reaches a hospitable endometrium. While this might sound simple enough, there are many factors that may prevent implantation from actually occurring. There are also actions you can take to support the chances of implantation occurring.

We have put together a 14-day guide to help you get through the TWW with steps you can take each day to support your uterine lining and increase your chances of implantation & pregnancy.
What can you do to increase your chances of implantation?
A healthy uterine lining is one of the factors needed for implantation to occur. There are a few measures you can take, regardless of whether this is a natural round or you have proceeded with a method of assisted reproduction (medication, IUI, IVF), to encourage a healthy uterine lining.
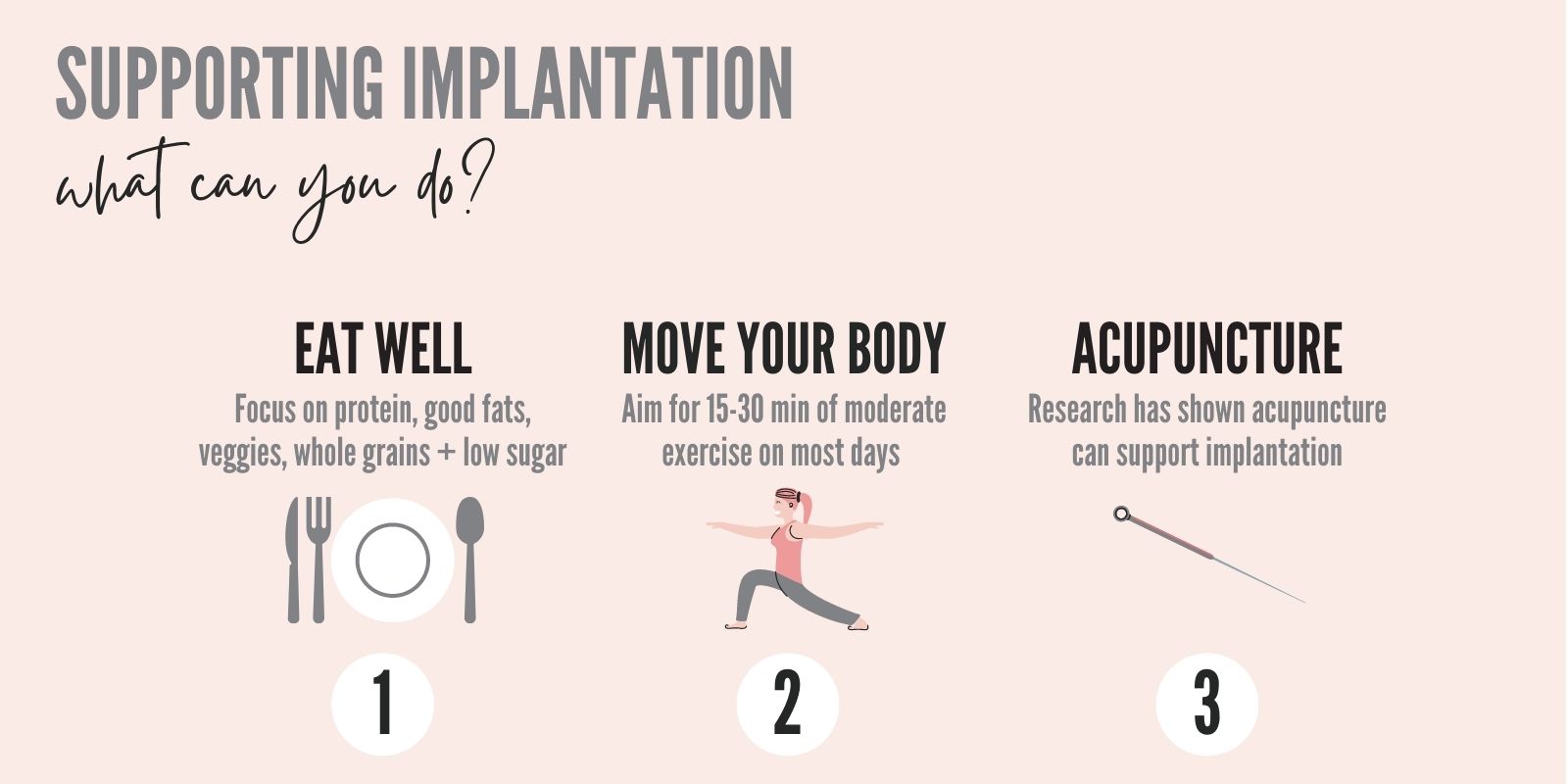
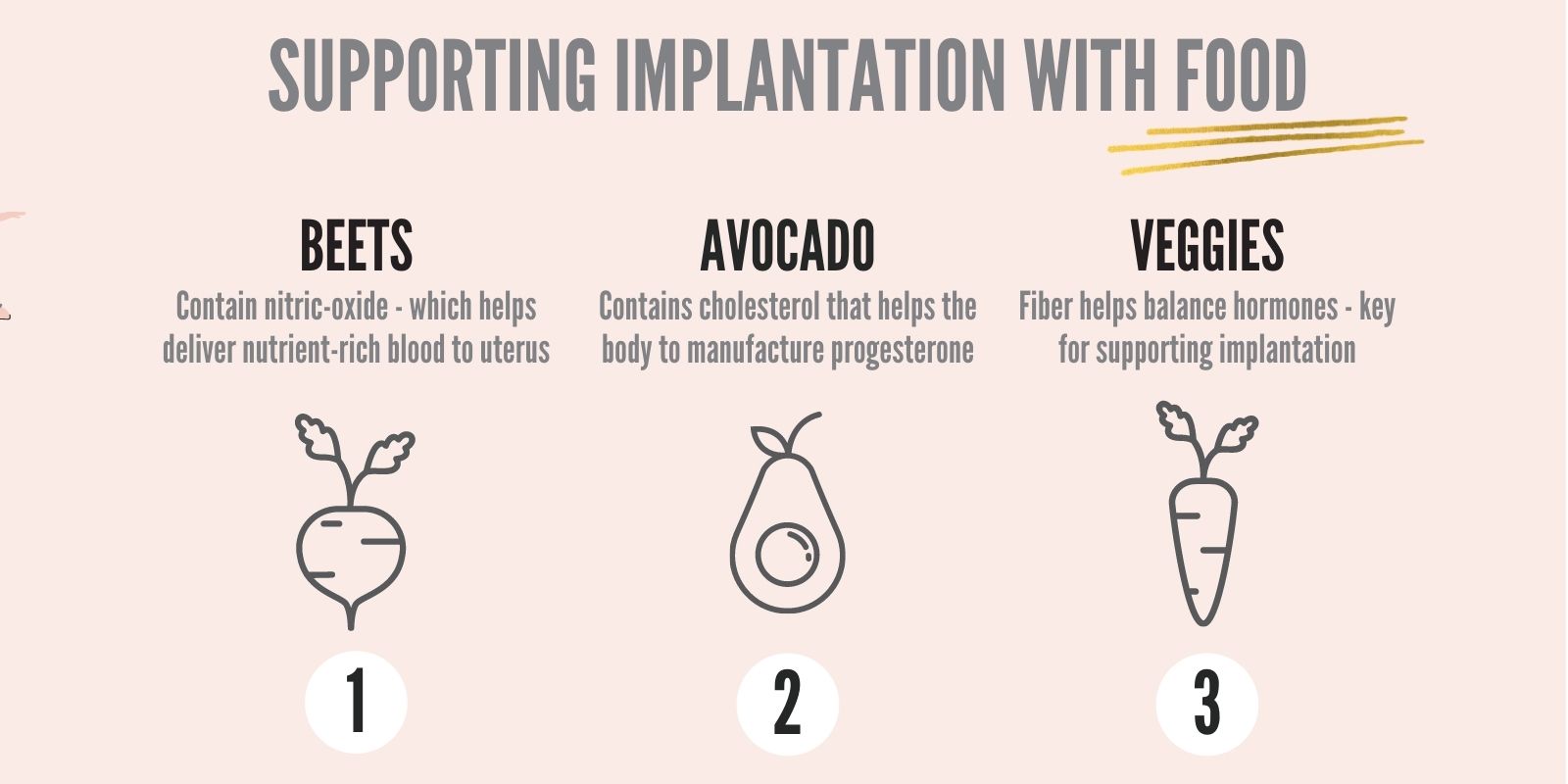
- Eat well: this is a particularly important time to ensure you are properly nourishing your body. Research has shown diets rich in good fats, a variety of vegetables, protein, whole grains, and unprocessed, low-in-sugar foods can help support fertility. Some of the key factors that influence implantation include balanced hormones, an anti-inflammatory environment, healthy progesterone levels (see the blog on Luteal Phase for more info on this), and so we need to make sure there are foods that support these things.
Consider:
Plant-based fats like avocado help provide that anti-inflammatory environment
Beets, one study showed that “beetroot contains nitric oxide, which dilates blood vessels allowing a rich supply of oxygenated, nutrient-rich blood to flow to the uterus…”
Bump up your vitamin C foods- these include citrus, bell peppers, and broccoli. One study showed that women who take Vit C had higher levels of progesterone.
Proteins like organic eggs and hemp also help to balance blood sugars and hormones. Both are vitally important for not only conception but also creating that optimal uterine environment.
- Move your body: incorporating regular, moderate exercise and activity into your routine encourages healthy, oxygenated blood flow to major organs – including your uterus.
What does this look like? Trying to fit in 15-30 minutes of exercise on most days of the week at a level you can talk, but not sing, at.
Some ideas? A brisk walk, your favorite workout video, or a nice bike ride – all great options! If you need help incorporated fertility-friendly exercise into your diet, get support here.
- Consider acupuncture: research has shown acupuncture may support fertility. Some women also find acupuncture to be very relaxing – so a win-win!
So why doesn’t implantation always occur?
There are two main reasons implantation may not occur in any given cycle:
- The uterus is not receptive to implantation
- There is an issue with the blastocyst
While advancements have been made in understanding human implantation, the detailed causes of implantation are quite numerous and not well known. For now, we will look at what is known.
Why might the uterus not be receptive to implantation?
- Structural challenges: if the uterus has scar tissue, endometriosis, polyps, or fibroids implantation rates may be affected
- Endometrium lining: research results vary on this topic, but some studies have demonstrated that a lining thickness of 8mm is ideal for implantation to occur; if the lining is too thin researchers have speculated this may lead to implantation failure although studies have shown pregnancy success even with “thin” linings
- Timing: there is a specific window of time, guided by hormonal and molecular signals, that promotes implantation – if hormones surge too early or late, or the right molecular signal cascade does not occur, implantation may be affected
- Infection: researchers have hypothesized that an infection in the uterus may impact implantation
- Immunological theories: research in this area continues to investigate immunological factors behind implantation failure
What could be wrong with the fertilized egg?
The fertilized egg plays an important role in implantation. As it continues to grow and divide from the blastocyst stage it becomes ready to “stick” to the endometrium by exposing a later of “sticky” cells. It also “communicates” with the uterine lining by sending signals that tell the uterine lining to prepare for arrival. All of these activities are controlled by the genetics of the fertilized egg. If there is a genetic abnormality the genes that contain the “instructions” to carry out any of these tasks might not be present or work properly, and that could lead to a failure to implant.
How do you improve the chances of a genetically normal blastocyst?
Good quality gametes (eggs & sperm) having a higher likelihood of leading to good quality blastocysts. For a closer look at improving egg quality read this. If you are proceeding with IVF there are a number of factors the lab and your medical team take into account to support a healthy embryo and you can ask your doctor which approach is recommended for your particular care.
Going through fertility treatments? Read on!
If you are going through fertility treatment (medicated cycle, IUI, or IVF) your doctor may prescribe a variety of different medications. These may include a blood thinner (like Aspirin), a steroid, utilize immunotherapy, or a range of other options.
Two “hot topics” in the realm of implantation and uterine receptivity are embryo glue and endometrial receptivity assays (ERA). Let’s take a closer look at each.
What is embryo glue?
Not something you can grab at your local craft store, but rather it is a solution that contains hyaluronan, a substance naturally produced in your body. It acts as your natural uterine secretions to help make the embryo “stickier”. Before an embryo transfer, the embryo is placed in the solution and then transferred to your uterus. Research on this medium is ongoing. Some studies have shown higher pregnancy rates with patients who had the glue incorporated into the embryo transfer, but these results were not statistically significant. Nonetheless, the cost is minimal and risks are negligible and so some clinics offer it as an option to patients.
What is an endometrial receptivity assay?
An endometrial receptivity assay, or ERA, is another testing option available to patients who experience repeated implantation failure following IVF embryo transfers.
How does ERA work?
The patient goes through a mock cycle – that is, a cycle like that of an embryo transfer without the actual transfer. Instead of transferring an embryo, the doctor will take a small biopsy of the patient’s uterine lining. The sample is used to profile the patient’s individual genetic expression of proteins. This helps to understand if the patient is receptive to implantation during the standard window of implantation, or if they have an altered window. Research is still ongoing in this field, but preliminary studies state “ERA is the most objective and accurate test available today for diagnosing endometrial receptivity”.
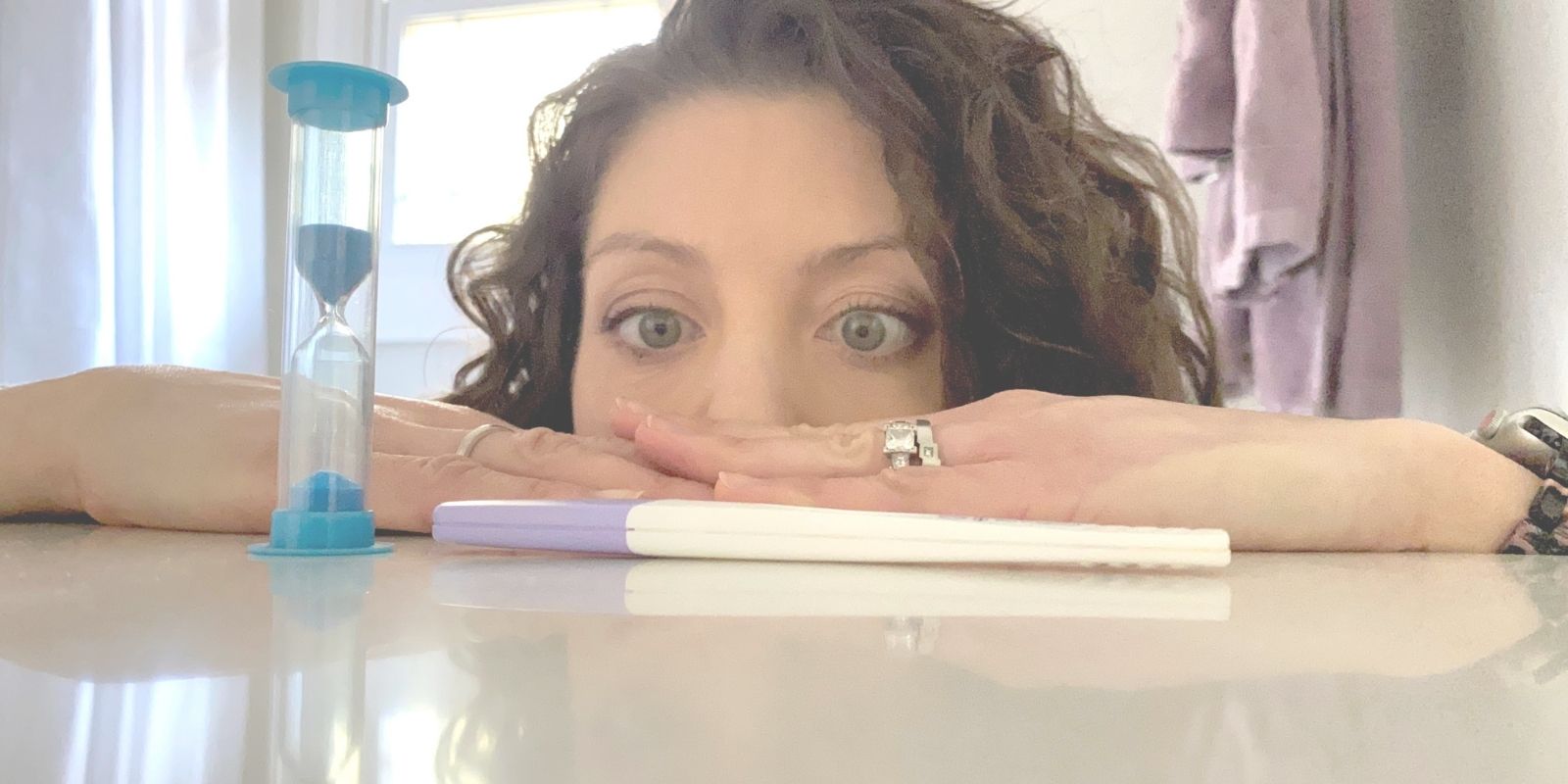
The two-week wait
So now you know what it takes for implantation to occur: what role your uterine lining plays, what role the fertilized egg plays, and some options to support success. All that’s left now is to wait those agonizing two weeks until your pregnancy test. For tips on surviving those 14 long days check out our article on Surviving the Two Week Wait.
Looking for early pregnancy signs?
The Mayo Clinic reports these early signs to look out for. But remember – these symptoms can be experienced without pregnancy – and you may also be pregnant without any of these symptoms.
- nausea
- sore breasts
- fatigue
- constipation
- spotting (also known as implantation bleeding*)
- cramping
- bloating
- food aversions
- missed period
*Implantation bleeding usually occurs before you would expect your period, only lasts 1-2 days. This is generally light in flow and is usually pinkish-brown versus red.
Take control of this cycle!
We have created a 14-day guide for your two-week wait. It’s loaded with tips to help increase your chances of implantation – grab it here!